Do Women Sleep Differently? Why Science Says Yes 😴
Sleep is a universal human need, but its patterns and quality are anything but the same. While we all require comfort to work, an increasing body of scientific research indicates that the way men and women experience sleep are different. These differences are not just anecdotes; They are inherent in a complex difference of biology, hormones and social factors. From the duration of sleep to the risk of some sleep disorders, scientific evidence pointed to a clear “yes” – in fact, sleep differently than men.
The Biological Blueprint: Hormones and the Sleep-Wake Cycle
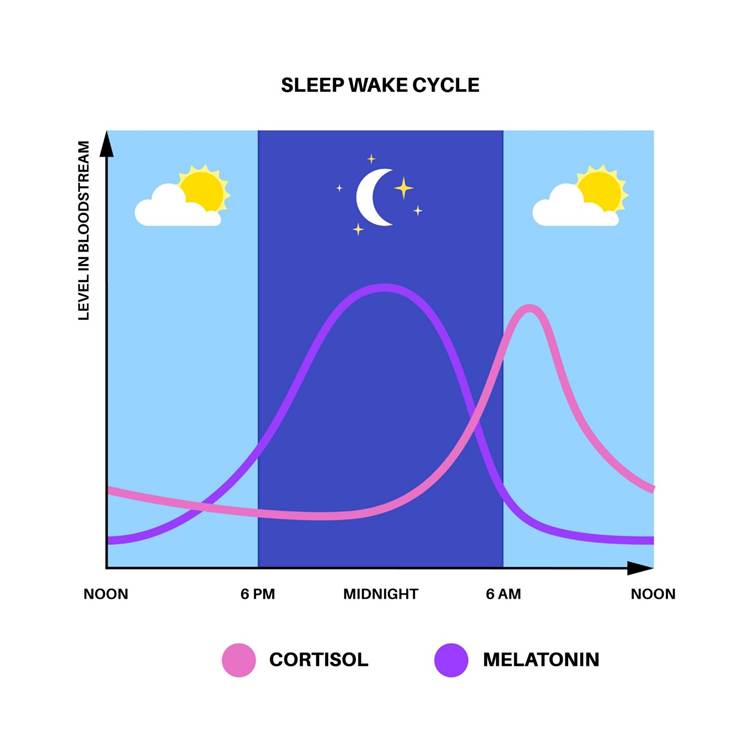
The most important factor running in sleep between men and women is hormonal ups and downs. During the life of a woman, her body undergoes a major hormonal shift that directly affects her sleepy cycle, or circadian rhythm.
- Menstruation: A woman’s menstrual cycle is a roller coaster of hormonal changes. For menstruation and during the first few days of its period, during the level of progesterone and estrogenic drops. This can cause symptoms such as cramps, inflammation and mood, which can all disrupt sleep. The report of many women increased the difficulty in sleeping and sleeping during this phase. Hormonal changes can also cause an increase in body temperature, making it difficult to flow.
- Pregnancy: Pregnancy is the duration of intensive hormonal changes, especially the increase in progesterone. While progesterone is often called “sleep hormones” because due to its sedative effects, its dramatic growth, combined with physical discomfort such as morning disease, persistent urination, and back pain, can severely slice sleep. A study published in the Sleep Journal found that pregnant women often experience low sleep duration and low sleep efficiency, especially in the third trimester.
- Menopause: Infection for menopause is marked by a decline in estrogen and progesterone. This hormonal shift is a major disruptive of sleep. The drop in estrogen is often associated with warm glow and night sweat, which can wake a woman from deep sleep, making her feel tired and may be disgusting the next day. A significant number of women after menopause and menopause reports to suffer from insomnia, as their body struggles to regulate temperature and maintain a consistent sleep.
Sleep Architecture: A Deeper Look at Sleep Stages
Beyond the amount of sleep, the quality and structure of sleep also varies between the sexes. Sleep is made up of several stages, including light sleep, deep sleep (slow sleep or SWS), and REM (Rapid Eye Movement) sleep.
- More deep sleep for women (mostly): Research indicates that women, on average, get more deep sleep than men. Deep sleep is the most restructure phase of the sleeping cycle, significant, cellular regeneration for physical repair, and strengthening the immune system. This may be a reason that women often report to feel more refreshed with less sleep than men. However, it is more prevalent in younger women and changes with age and hormonal shifts.
- Beginning of first and low sleep: Studies have shown that women have a strong drive to sleep first in the evening than men. This is likely to be slightly lower of their circadian rhythm. Women may feel tired even before, which can affect their bedtime and overall sleep routine.
The Disparity in Sleep Disorders
While both men and women can suffer from sleep disorders, there are remarkable differences in circulation and type.
- Insomnia: Women are more likely to diagnose insomnia than men. It is often associated with the first mentioned hormonal ups and downs, but also has a high proliferation of conditions such as stress, anxiety and depression, which can all contribute to sleep.
- Restless leg syndrome (RLS): This neurological disorder, which is characterized by an uncontrollable urge to move the feet, is more common in women, more common in women, with some studies suggest that men are almost doubled in men. RLS can be particularly disruptive for gold, making it difficult to fall and sleep. The condition can also be increased during pregnancy.
- Obstructive Sleep Apnea (OSA): Traditionally, OSA is usually more diagnosed in men. However, this can be caused by misconceptions about its symptoms. While men with OSA are often present with loud snoring, women’s symptoms can be more subtle and etipical, such as fatigue, headache, or mood disturbances, which lead to wrong diagnosis. The risk for women increases after menopause.
Societal and Lifestyle Factors
This would be an oversmimphalification to fully characterize all sleep differences for biology. Social roles and lifestyle factors also play an important role in how women sleep.
- “Second innings”: Many women still carry primary responsibility for domestic duties and childcare, even when they work full -time. This “second innings” often involves late night tasks, such as feeding a child, tendering to a sick child, or finishing the work after all the rest go to bed. This unpaid labor can lead to lack of chronic sleep. A study published in Journal Science Advance found that mothers are more likely to be fragmented sleep than father.
- Stress and mental weight: Women, on average, report high levels of stress than men. This stress can be the result of many roles, professional pressures and emotional labor of management of family and social relationships. High stress levels are directly associated with cortisol production, stress hormones, which can make it difficult to relax and sleep.
- Social expectations: There is a social hope that women must be “on” and available, both professional and personally. This can lead to a tendency to sacrifice sleep to meet these expectations, leading to a cycle of sleep deficiency.
The Brain’s Role in a Restless Night
The difference in sleep between men and women is also associated with brain function. Research has shown that women’s brains are more connected between the two hemispheres, which some scientists believe that multitask’s greater capacity and an increased level of emotional processing may contribute. While it has its own benefits, it can also take inability to “close” the brain at night, making it difficult to sleep. Women’s brains are also more sensitive to light and noise during sleep, making them more easily awakened than external stimuli.
Conclusion: A Call for Gender-Specific Sleep Solutions
The evidence is clear: Women sleep separately than men due to a combination of hormonal, organic and social factors. It is not about a sex, which is a “better” sleeper than the other, but about recognizing the unique challenges faced by women in achieving quality comfort. Understanding these differences is the first step towards finding a solution. This may include gender-specific approaches to treat sleep disorders, considering hormonal health in sleep recommendations, and advocating more equitable division of labor at home. As science keeps highlighting the complications of sleep, it becomes clear that a size-fit-all approach is not effective. In fact, to promote public health, we must accept and address the unique sleep needs of both men and women.